Is Mammography Radiation Safe?
Mammograms are one of the most effective tools for detecting breast cancer early, but the question of radiation exposure is a common concern. How much radiation do mammograms actually involve? Is it safe? And how does it compare to the radiation we’re exposed to in daily life? Here, our team at Breast Imaging Victoria explores these questions, providing clear, reassuring answers to help you make informed decisions about your breast health.
How Much Radiation Does a Mammogram Use?
A standard 2D mammogram typically uses 0.4–0.5 mSv (millisieverts) of radiation, while a 3D mammogram (tomosynthesis) uses slightly more, ranging from 0.5–1 mSv. To put these numbers into perspective, the average Australian is exposed to 1.5–2 mSv of natural background radiation annually, according to ARPANSA (Australian Radiation Protection and Nuclear Safety Agency).
These doses are considered very low. To illustrate:
2D Mammogram: 0.4–0.5 mSv
3D Mammogram: 0.5–1 mSv
Annual Background Radiation (Australia): 1.5–2 mSv
A Short Flight (e.g., Melbourne to Sydney): 0.02–0.05 mSv
A Long Flight (e.g., Melbourne to London): 0.11 mSv
This comparison shows that a mammogram involves a similar radiation dose to just a few months of natural background exposure or a long-haul flight.
Why Mammogram Radiation is Considered Safe
1. The ALARA Principle
Australia follows the ALARA principle (As Low As Reasonably Achievable) to minimise radiation exposure without compromising the quality of the images. This ensures every mammogram is conducted with the smallest dose necessary to achieve accurate results.
2. Life-Saving Benefits
The small amount of radiation from a mammogram pales in comparison to the life-saving potential of early breast cancer detection. Identifying cancer early often means less invasive treatment, better outcomes, and increased survival rates.
3. Advanced Technology and Expertise
Modern mammography machines are designed to deliver high-quality images with minimal radiation. Radiographers are extensively trained to position patients correctly and reduce the need for repeat imaging, further limiting exposure.
Everyday Radiation: Putting Mammograms in Perspective
Radiation is all around us—naturally occurring in the air, soil, and even some foods. Here’s how mammogram radiation compares to other common exposures:
| Source | Radiation Dose (mSv) |
|---|---|
| 2D Mammogram | ~0.4–0.5 |
| 3D Mammogram | ~0.5–1 |
| Annual Background (Australia) | ~1.5–2 |
| Short Flight (Melbourne to Sydney) | ~0.02–0.05 |
| Long Flight (Melbourne to London) | ~0.11 |
Seeing these numbers side by side helps demystify mammogram radiation. It’s a small dose when compared to the exposure we encounter in our everyday lives!
Balancing Risks and Benefits: The Bigger Picture
It’s natural to feel apprehensive about any medical procedure involving radiation. However, the risks associated with mammogram-level radiation are extremely low, especially when weighed against the significant benefits:
Early Detection Saves Lives: Mammograms often catch breast cancer in its earliest stages, allowing for more effective treatments.
Low and Controlled Doses: The radiation exposure is brief and tightly regulated to ensure safety.
Personalised Care: Radiographers and radiologists tailor each procedure to your specific needs, using the latest equipment and techniques to optimise accuracy and minimise risk.
If you have concerns, remember that discussing them with your healthcare provider can help clarify any doubts.
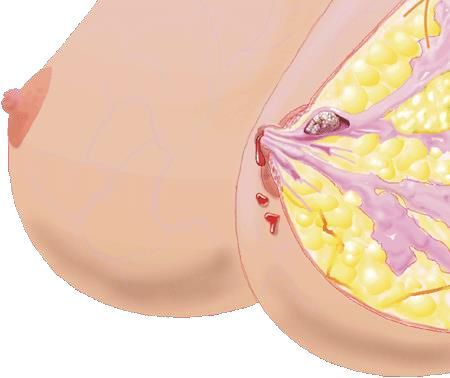
Breast Imaging Beyond Mammograms
Not all breast imaging involves radiation. Here’s a breakdown of common breast imaging and assessment technologies:
How It Works: Uses sound waves to create images of the breast tissue.
Radiation: None.
When It’s Used: To evaluate cysts, guide biopsies, or examine dense breast tissue.
2. MRI (Magnetic Resonance Imaging)
How It Works: Relies on magnetic fields and radio waves.
Radiation: None.
When It’s Used: For high-risk patients or when more detailed imaging is required.
3. Contrast-Enhanced Mammography (CEM)
How It Works: Combines low-dose X-rays with an iodine-based contrast agent to enhance image clarity.
Radiation: Slightly higher than standard mammography but still within regulated safe ranges.
When It’s Used: For cases requiring more detailed imaging, often when a patient has more dense breast tissue.
Your radiologist will recommend the most suitable imaging method based on factors such as breast density, medical history, and clinical findings.
Making Informed Choices About Your Breast Health
Understanding the safety of mammography can help ease concerns and empower you to take a proactive approach to managing your breast health. Here are some key points to keep in mind when considering a mammogram:
Radiation Is Minimal: The amount of radiation used in a mammogram is comparable to just a few months of natural background exposure. This low dose is carefully regulated to provide the clearest images possible while prioritising your safety.
Benefits Are Substantial: Early detection through mammography can make a significant difference in outcomes. Catching breast cancer in its early stages often leads to more treatment options, less invasive interventions, and a higher likelihood of a successful recovery. For instance, the five-year survival rate is nearly 100% for Stage 1 breast cancer, 95% for Stage 2, 81% for Stage 3, and drops to 32% for Stage 4.
Safety Is a Priority: Mammograms in Australia adhere to strict safety protocols guided by national standards. Advanced imaging technology and well-trained radiographers ensure that the process is both safe and effective, with minimal risk to patients.
Tailored Screening Recommendations: Mammograms are not one-size-fits-all. Your healthcare provider will tailor screening recommendations based on factors such as your age, family history, and personal risk level, ensuring that your breast health plan is customised to your needs.
Holistic Care Options: Mammography is just one part of breast health management. Other imaging modalities, such as ultrasound or MRI, may be recommended based on your breast density or clinical findings. Working with a trusted radiologist ensures you receive the right care.
Accessible Resources: Many clinics provide additional support, such as online resources, comparison reports, and follow-up care. These services can help you understand your results and next steps, offering peace of mind.
Your breast health is vital, and so is your peace of mind. If you have questions or concerns, reach out to a trusted healthcare provider who can guide you through the process and ensure you feel confident in your decisions.
Your Health Comes First!
Mammograms are a vital tool in the fight against breast cancer. By balancing minimal risks with significant benefits, they empower individuals to take charge of their breast health with confidence. Whether you’re due for your first mammogram or have questions about other imaging options, rest assured that today’s technology and practices prioritise your safety and well-being.
For more information, reach out to our teamat Breast Imaging Victoria or book your next mammogram. Early detection makes all the difference. Let’s prioritise your health together!
FAQs
1. Is it okay to have multiple mammograms in a year if needed?
Yes, it is safe to have multiple
mammograms if clinically necessary. The radiation doses are low and carefully controlled, so the benefits of accurate diagnosis and early detection far outweigh the minimal risks. Frequent imaging may be recommended when monitoring changes or following up on suspicious findings.
Your healthcare provider will only suggest additional mammograms if they are vital to your care, ensuring the process remains safe and beneficial.
2. Can I choose an ultrasound or MRI instead of a mammogram?
Whether abreast ultrasound or MRI is appropriate depends on your individual situation, such as breast density, medical history, and symptoms. Mammography is typically the first choice because it effectively detects early signs of breast cancer. However, ultrasound, Contrast Enhanced Mammogram (CEM), or MRI may be used as supplementary tools for further evaluation or in specific cases, for example, if you havedenser breast tissue or high-risk factors. Your radiologist will recommend the best imaging method for your needs.
3. Is mammography safe during pregnancy or breastfeeding?
Mammography is generally avoided during pregnancy unless it is absolutely necessary. Ultrasound is a preferred alternative during this time because it doesn’t involve radiation. For breastfeeding individuals, mammography can often be safely performed, but it’s important to discuss your situation with your healthcare provider. They will assess your specific needs and recommend the safest and most effective imaging option to protect both you and your baby while addressing your breast health.
4. How can I be sure mammogram machines are safe?
Mammogram machines in Australia must meet strict safety standards regulated by ARPANSA and state authorities. These machines are regularly tested and maintained to ensure they deliver low radiation doses while producing high-quality images. Radiographers are trained to use the equipment properly, prioritising your safety during the procedure. By adhering to these rigorous protocols, mammogram providers in Melbourne minimise risks and maximise diagnostic accuracy, ensuring you receive safe and effective breast imaging care.
5. Does radiation exposure from mammograms accumulate over time?
Yes, radiation exposure does accumulate over a lifetime, but the doses from mammograms are so low that the overall risk remains minimal. In fact, a 2D mammogram uses 0.4–0.5 mSv of radiation, 3D mammograms use 0.5–1 mSv, compared to 1.5–2 mSv of annual natural background radiation in Australia! The benefits of early cancer detection far outweigh any potential risks associated with cumulative exposure. Mammography is designed to provide crucial diagnostic information while keeping radiation levels as low as possible. If you have concerns, speak with our breast imaging clinic in Melbourne, who can address your questions and tailor screening recommendations to your needs.
CONTACT
Level 4
21 Victoria Street
Melbourne VIC 3000
Fax: (03)
9492 3600
Fax: (03)
9492 3600
Hours:
Mon – Fri: 8.00am - 4.00pm
Closed weekends and public holidays.
Hours:
Mon – Fri: 8.00am - 4.00pm
Closed weekends and public holidays.
CONTACT US
We will get back to you as soon as possible.
Please try again later.