Fibroadenoma
Benign Breast Conditions: Meet the Fibroadenoma
Did you know that not all lumps or abnormalities found in breast tissue are cause for immediate concern? Today, we’re shedding light on a common benign (non-cancerous) breast condition known as a Fibroadenoma, often whimsically referred to as a "breast mouse."
What is a Fibroadenoma?
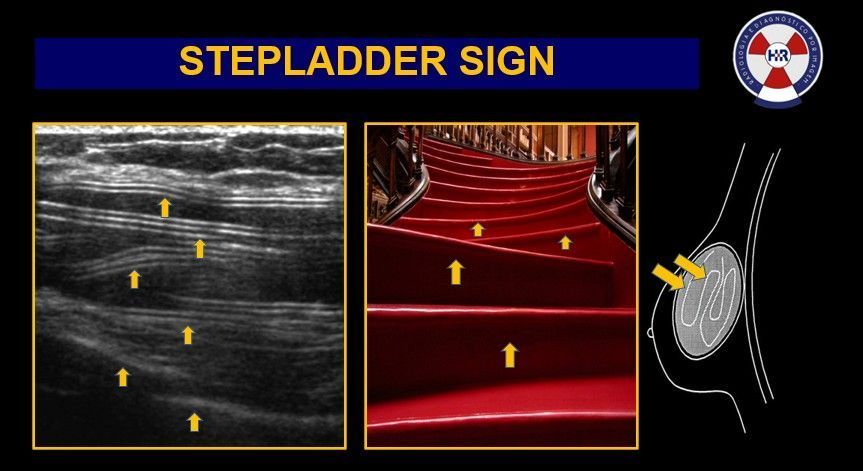
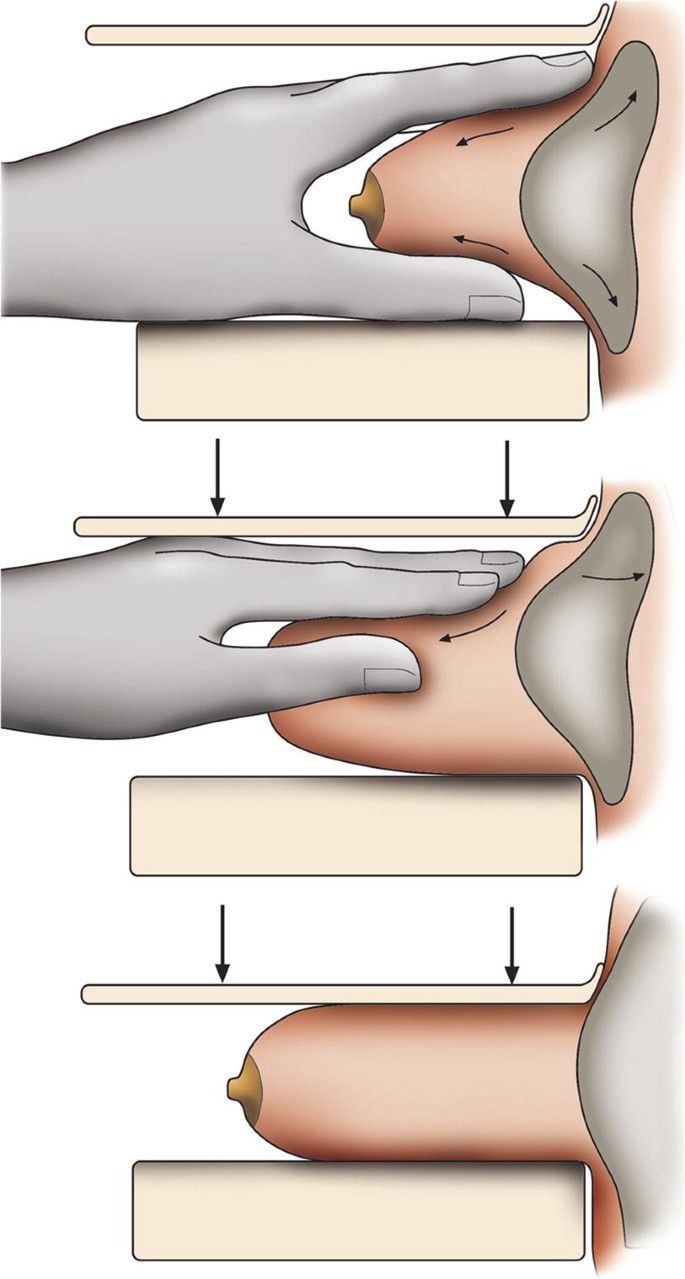
Fibroadenomas are solid, smooth, and firm benign tumours that are most common in women between the ages of 15 and 35. They get their nickname, "breast mouse," from their ability to move easily within the breast tissue when touched, much like a mouse scurrying under a rug.
What Causes Fibroadenomas?
The exact cause of fibroadenomas isn't fully understood, but they're closely linked to hormonal changes in the body. These benign tumours are most common during a woman's reproductive years, suggesting that estrogen plays a significant role in their development. Fibroadenomas can vary in size during the menstrual cycle, pregnancy, and breastfeeding, reflecting the influence of hormonal levels. While they are influenced by the body's hormonal environment, they are generally considered to be low risk in terms of breast cancer development.
Characteristics of Fibroadenomas:
- Size: They can range from as small as a marble to as large as a golf ball.
- Shape: Typically round or lobular, with distinct edges that sometimes can be felt through the skin.
- Feel: They are usually painless, but their presence is usually palpable and can sometimes increase in size with hormonal changes, such as during menstruation.
Why it Matters:
Understanding the nature of fibroadenomas is crucial for peace of mind and informed health decisions. While they are benign, monitoring is essential to observe any changes in size or feel, as part of routine breast health management.
Diagnosis and Management:
Fibroadenomas are usually diagnosed through clinical examination, ultrasound, or a mammogram and can be confirmed with a biopsy. In most cases, they don’t require treatment and may shrink on their own. It is very common to get many of them in one breast or both! However, if a fibroadenoma is large, is growing quickly or causes discomfort, it can be surgically removed.
Remember:
Regular breast screenings and being familiar with how your breasts normally look and feel are key components of breast health. If you notice any changes or new lumps, it's important to consult with a healthcare provider.
Breast Imaging Victoria is here to support your journey towards understanding and managing your breast health. For more information or to schedule a breast scan, reach out to us today.